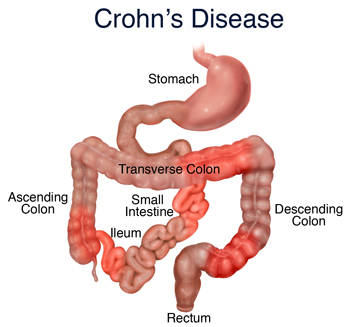
While studies have shown that food allergies are not the cause of Crohn’s disease, most agree that they can have a direct affect on flare-ups that do occur. Like other triggers, food allergies can exacerbate the already tender intestinal lining causing severe inflammation that can have long-term problems if it’s a continued problem.
Defining Allergy
There are several ways to determine if you are sensitive to certain foods. Your doctor can order a series of blood tests much like those given to determine allergies to cats, dogs, and bees.
Keep in mind that these tests only show which foods have an immunity reaction by the body, which is the technical definition of food allergies. For the purposes of this discussion, however, we will be referring to food sensitivities and food allergies interchangeably, as both can and will cause serious problems to someone with an IBD.
Because of this, it is important to find another way to determine which are the most common food allergens, and whether or not they directly affect you.
Most Common Food Allergens
Many types of foods can cause an adverse reaction to the intestines, but there are some that have proven more difficult to digest than others, and in fact have caused such severe allergic reactions as to cause death in come cases. The following list is not exhaustive, but does provide the most common foods found to be a problem:
- Eggs
- Peanuts and other tree nuts
- Fish and Shellfish
- Milk and Lactose
- Wheat and Gluten
- Soy products
- Corn
Other food sensitivities can include spicy foods like barbeque sauce or salsas, gassy foods like cabbage and broccoli, and difficult to digest foods like red meat and deep-fried foods.
Determining for Yourself
Since doctors rely on blood tests to determine allergies, and not sensitivities, if falls on the individual to discover what are the more painful types of things to him or her personally. Here is an easy, direct way to figure this out:
- First, during a remission, remove all “dangerous” foods from your diet. Stay on a bland, soft-food menu for two weeks to allow the other foods to leave your system.
- Second, add one new type of food to your menu at a time, allowing a week per food to decide if it is an irritation to your system.
- As you find your personal irritants, keep a list. Post it in the kitchen for easy access when grocery shopping, and when reaching for a snack.
- Go through the process again during a flare-up to determine which of your “safe” foods aren’t so safe when you’re already in pain.
Remember that it is best to try this during a remission, as some food may be perfectly fine normally, but impossible during a flare-up.
Once you have determined your safe foods, write them down on a small piece of paper that you can keep with you at all times. This makes going to a party or out to eat much easier, as you can refer to the list before eating something you that might later cause a good deal of pain.